Providers FAQs View Global FAQs
22 results
-
About Empower
What is Empower Healthcare Solutions (Empower)?
Empower is one of four PASSE organizations in the state. We empower individuals to lead fuller, healthier lives at home and in their communities. PASSE (Provider-Led Arkansas Shared Savings Entity) is a Medicaid program to address the needs of individuals who have intensive behavioral health, intellectual disability, or developmental disability service needs.
Why is the PASSE program good for my patients?
The goal of the PASSE model is to improve the health of Arkansans who need intensive levels of specialized care due to behavioral health issues or developmental/intellectual disabilities. The PASSE model includes Care Coordination, which coordinates care for all community based services to improve total health outcomes for these members.
-
About Empower Benefits and Services
What type of services are covered for Empower Members?
Empower members will be eligible for all services covered under the Medicaid state plan, as well as Section 1915(i) and CES waiver services, including therapy services and services through the Early Periodic Screening Diagnosis and Treatment (EPSDT) program for children. In short, members will have access to services covered under the Medicaid program today, as long as those services are deemed medically necessary and documented in the member’s Person Centered Service Plan (PCSP).
How do Empower Members get a Primary Care Provider?
Members select their PCP when they sign up for Medicaid. Members who are also eligible for Medicare are able to keep their Medicare PCP. For any members who do not select a PCP, Empower will automatically assign a PCP based on:
- the member’s claims history (who they have seen in the past);
- a member’s geographical location;
- appropriate distribution by provider (so that members are not overly concentrated with the same PCP).
Members ages 18 and older will be assigned to a general or family practitioner, internal medicine, or other specialty provider approved by the state. Members under 18 years old will be assigned to a pediatrician or family practitioner. At any time, a member can call Empower Member Services and request that their PCP be changed, and Empower will honor that request if they are an In-Network provider.
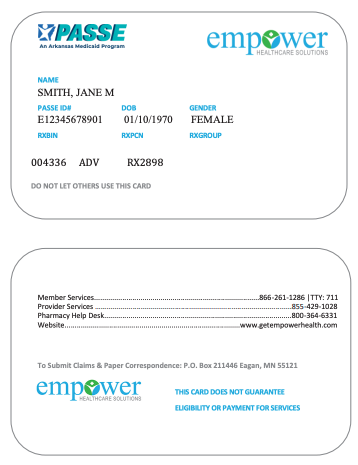
How do I know if an individual is a member of Empower?
All Empower members will have a member ID card. Members should always present their ID at the time of service, but an ID card, in and of itself, is not a guarantee of eligibility. Providers must verify a member’s eligibility on every date of service.

The ID card will contain the following information:
- Member’s name, Date of Birth, and Gender
- PASSE ID number
- Pharmacy ID number
- Empower contact information
- Claims filing address
How do I verify Member Eligibility?
Empower member eligibility may change daily. Therefore, each participating provider is responsible for verifying eligibility with Empower before providing services to a member. Providers may verify eligibility using the following methods:
- Online – Visit our Business Operations Portal
- Telephone – Contact Provider Services at 1-855-429-1028.
-
Care Coordination and Quality
Will I be required to report any quality measures for Empower?
Empower is committed to ensuring that continuous quality/performance improvement occurs. There is consistent and ongoing monitoring for applicability so Empower can achieve efficiency and effectiveness with improved outcomes for our members. HEDIS Measures will be used.
-
Cultural Competency & Member Rights
What are the rights of Empower Members?
Member Rights and Responsibilities are listed in the Member Handbook, available on the Empower website www.getempowerhealth.com.
-
Joining the Empower Network
Who can answer questions about my contract as an Empower Provider?
You can contact the Empower network team at [email protected] for help with questions about your Provider contract.
How can I get a copy of the Empower Provider Manual?
The provider manual is available electronically on the Empower website, www.getempowerhealth.com/for-providers/provider-materials/provider-handbook/.
What are my rights and responsibilities as an Empower Provider?
Provider Rights and Responsibilities are in the Empower Provider Handbook, found on the Empower website www.getempowerhealth.com/for-providers/provider-materials/provider-handbook/.
How do I join the Empower pharmacy network?
Empower is participating in the Caremark/CVS national network. If you are an AR pharmacy provider and in the Caremark/CVS national network then no action is needed. You can check the CVS national network here:
https://www.caremark.com/wps/myportal/PHARMACY_LOCATOR_FASTIf you are interested in joining the CVS network, you can start the process here:
https://www.caremark.com/wps/portal/FOR_HEALTH_PROS_HOME
Relevant links here include “Pharmacy Pre-Enrollment Questionnaire” and “Pharmacy Enrollment.”How can I join Empower as a provider?
To become a participating provider with Empower, please complete the Empower Network Application located at the Providers Page under Forms and Resources and email to [email protected]. If you have questions please contact Empower Provider Relations at 855-429-1028.
How do I update my roster?
To update your roster, please complete the Provider Roster Form located on the Providers page under “Provider Forms and Resources” and email to [email protected]. If you have questions please contact Empower Provider Services at 855-429-1028.
-
Prior Authorization/Utilization Management
I have additional questions about billing. Who can answer my questions and when can they answer them?
Empower’s Provider Services team will be available to help you via phone at 855-429-1028, Monday through Friday (except holidays), from 8:00 AM to 5:00 PM CT. You may also reach out to Empower’s Provider Relations Advocates for assistance by emailing [email protected].
How do I submit a claim and when can I submit a claim?
To make sure that Empower can process your claims in a timely manner, it is important that providers ensure Empower has accurate billing information on file. Providers must have a current, active Arkansas Medicaid Provider ID. Please confirm with Empower’s Network department ([email protected]) that the following information is current in our files:
- Provider name (as noted on current W-9 form)
- National Provider Identifier (NPI)
- Tax Identification Number (TIN)
- Taxonomy code
- Physical location address (as noted on current W-9 form)
- Billing name and addres
For additional claims and payment information, please see Empower’s Provider Billing page.
How and when can I access information electronically about Empower Members?
Empower’s Business Operations Portal is available 24/7 and allows providers to instantly access many tools and resources. Providers and their office staff can register for our secure Business Operations Portal in just a few easy steps.
- Go to www.getempowerhealth.com
- Choose Business Operations from the Provider Home Page or Provider drop down
- Click ‘here’ to register
- Choose ‘Providers Click here’
- Register for Portal access
- Contracted Providers complete the web registration form.
- Out of Network Providers click ‘here’ under Provider Information to complete Portal Access Request
Once registered, the secure portal will allow you to:
- Request and track authorizations
- Submit claims and view payment history
- Verify member eligibility
- Review InterQual Criteria
What is the process for submitting Pharmacy PAs, and what pharmacy services require a PA?
Empower is committed to providing appropriate, high quality, cost-effective drug therapy to all of our members. Empower works with providers and pharmacists to ensure that medications used to treat a variety of conditions and diseases are covered. The plan covers prescription drugs and certain over-the-counter (OTC) drugs when ordered by an Empower physician. The pharmacy program does not cover all medications. Some drugs have a generic equivalent or a brand-name drug from a different manufacturer that is covered. Some medications require prior authorization or have limitations on age, dosage, maximum quantities, or any combination of these.
Prior Authorization is necessary for some medications to establish medical necessity, and to ensure eligibility for coverage per State regulations, Federal regulations, or both. This may be due to specific Food and Drug Administration (FDA) indications, the potential for misuse or overuse, safety limitations, or cost- benefit justifications.
A PA is required for certain medications that are:
- Outside the recommended age, dose, or gender limits;
- Not listed on the Preferred Drug List (PDL);
- Listed on the PDL but still require Prior Authorization;
- Brand name drugs when a generic exists;
- A Duplication in therapy (i.e. another drug currently used within the same class);
- New to the market and not yet reviewed by the P&T Committee;
- Prescribed for off-label use or outside of certain diseases or specialties; or
- Self-injectable and infusion medications (including chemotherapy) with some exceptions.
Providers may request an exception to Empower’s PDL either verbally or in writing. For written requests, providers should complete a Prior Authorization Request Form that includes pertinent enrollee medical history and information. Prior Authorization Request Forms may be accessed on Empower’s Pharmacy Forms and Resources page.
If authorization cannot be approved or denied, and the drug is medically necessary, up to a 72-hour emergency supply of the drug can be supplied to the member.
How do I submit a Prior Authorization (PA) or an Extension of Benefits?
Providers may submit Prior Authorizations in the following methods:
- Online – Visit our Business Operations Portal at https://bharportal.valence.care/
- Telephone – Contact Provider Services at 1-855-429-1028. Select option 2 for Utilization Management.
What services require an Extension of Benefits?
Some services have yearly benefit limits available before an Extension of Benefits request is required. Please see Prior Authorization Resources on Empower’s Providers page and clicking “Provider Forms and Resources” for benefit limits.
What services require a PA?
Some services require a prior authorization from Empower for reimbursement to be issued. Please see Provider Forms and Resources on Empower’s website where there’s a link to a Quick Reference Guide for Key Contact Information and Prior Authorization for a list of services that require Prior Authorization.
-
Training
What training will be provided to me as a PASSE provider and when?
Please check Empower’s Providers page and click Provider Training regularly for upcoming trainings and educational opportunities.